Cervical Radiculopathy (Pinched Nerve)
Introduction
Cervical radiculopathy, commonly called a "pinched nerve" occurs when a nerve in the neck is compressed or irritated where it branches away from the spinal cord. This may cause pain that radiates into the shoulder, as well as muscle weakness and numbness that travels down the arm and into the hand.
Cervical radiculopathy is often caused by "wear and tear" changes that occur in the spine as we age, such as arthritis. In younger people, it is most often caused by a sudden injury that results in a herniated disk.
In most cases, cervical radiculopathy responds well to conservative treatment that includes medication and physical therapy.
Anatomy
Your spine is made up of 24 bones, called vertebrae, that are stacked on top of one another. These bones connect to create a canal that protects the spinal cord.
Animation courtesy Visual Health Solutions, Inc.
The seven small vertebrae that begin at the base of the skull and form the neck comprise the cervical spine.
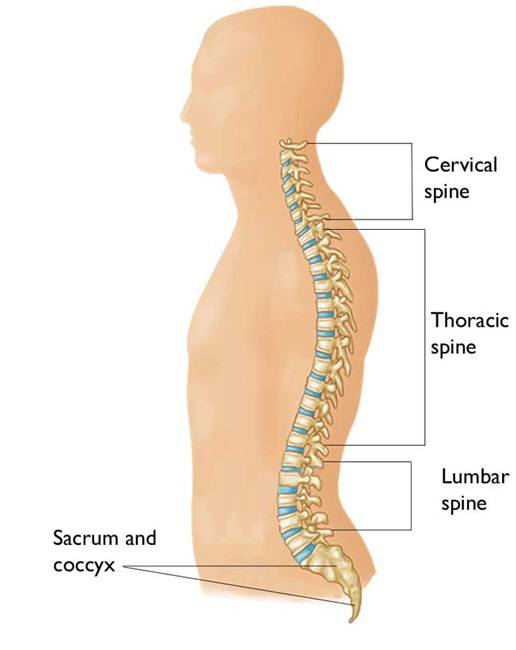
Cervical radiculopathy occurs in the cervical spine--the seven small vertebrae that form the neck.
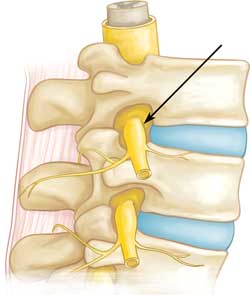
Spinal nerve root.
Other parts of your spine include:
Spinal cord and nerves. These "electrical cables" travel through the spinal canal carrying messages between your brain and muscles. Nerve roots branch out from the spinal cord through openings in the vertebrae (foramen).
Intervertebral disks. In between your vertebrae are flexible intervertebral disks. They act as shock absorbers when you walk or run.
Intervertebral disks are flat and round and about 1.3 cm thick. They are made up of two components:
- Annulus fibrosus. This is the tough, flexible outer ring of the disk.
- Nucleus pulposus. This is the soft, jelly-like centre of the disk.
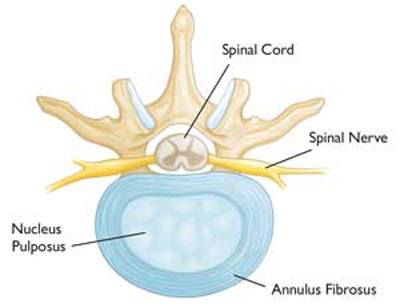
A healthy intervertebral disk (cross-section view).
Cause
Cervical radiculopathy most often arises from degenerative changes that occur in the spine as we age or from an injury that causes a herniated, or bulging, intervertebral disk.
Degenerative changes. As the disks in the spine age, they lose height and begin to bulge. They also lose water content, begin to dry out, and become stiffer. This problem causes settling, or collapse, of the disk spaces and loss of disk space height.
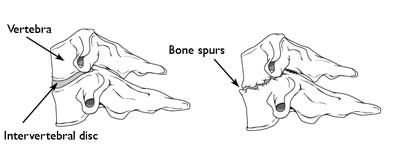
(Left) Side view of a healthy cervical vertebra and disk. (Right) A disk that has degenerated and collapsed.
As the disks lose height, the vertebrae move closer together. The body responds to the collapsed disk by forming more bone —called bone spurs—around the disk to strengthen it. These bone spurs contribute to the stiffening of the spine. They may also narrow the foramen—the small openings on each side of the spinal column where the nerve roots exit—and pinch the nerve root.
Degenerative changes in the disks are often called arthritis or spondylosis. These changes are normal and they occur in everyone. In fact, nearly half of all people middle-aged and older have worn disks and pinched nerves that do not cause painful symptoms. It is not known why some patients develop symptoms and others do not.

Herniated disk (side view and cross section)
Herniated disk. A disk herniates when its jelly-like centre (nucleus) pushes against its outer ring (annulus). If the disk is very worn or injured, the nucleus may squeeze all the way through. When the herniated disk bulges out toward the spinal canal, it puts pressure on the sensitive nerve root, causing pain and weakness in the area the nerve supplies.
A herniated disk often occurs with lifting, pulling, bending, or twisting movements.
Symptoms
In most cases, the pain of cervical radiculopathy starts at the neck and travels down the arm in the area served by the damaged nerve. This pain is usually described as burning or sharp. Certain neck movements—like extending or straining the neck or turning the head—may increase the pain. Other symptoms include:
- Tingling or the feeling of "pins and needles" in the fingers or hand
- Weakness in the muscles of the arm, shoulder, or hand
- Loss of sensation
Some patients report that pain decreases when they place their hands-on top of their head. This movement may temporarily relieve pressure on the nerve root.
Doctor Examination
Physical Examination
After discussing your medical history and general health, your doctor will ask you about your symptoms. He or she will then examine your neck, shoulder, arms and hands—looking for muscle weakness, loss of sensation, or any change in your reflexes.
Your doctor may also ask you to perform certain neck and arm movements to try to recreate and/or relieve your symptoms.
Tests
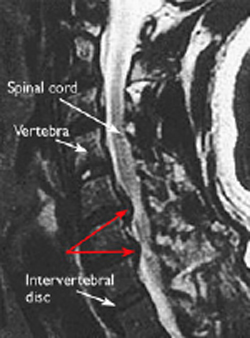
This MRI image shows bulging disks pressing on the spinal cord (red arrows). Reproduced from Boyce R, Wang J: Evaluation of Neck pain, radiculopathy and myelopathy: imaging, conservative treatment, and surgical indications. Instructional Course Lectures 52. Rosemont, IL, American Academy of Orthopaedic Surgeons, 2003, pp 489-495.
X-rays. These provide images of dense structures, such as bone. An x-ray will show the alignment of bones along your neck. It can also reveal whether there is any narrowing of the foramen and damage to the disks.
Computed tomography (CT) scans. More detailed than a plain x-ray, a CT scan can help your doctor determine whether you have developed bone spurs near the foramen in your cervical spine.
Magnetic resonance imaging (MRI) scans. These studies create better images of the body's soft tissues. An MRI of the neck can show if your nerve compression is caused by damage to soft tissues—such as a bulging or herniated disk. It can also help your doctor determine whether there is any damage to your spinal cord or nerve roots.
Electromyography (EMG). Electromyography measures the electrical impulses of the muscles at rest and during contractions. Nerve conduction studies are often done along with EMG to determine if a nerve is functioning normally. Together, these tests can help your doctor determine whether your symptoms are caused by pressure on spinal nerve roots and nerve damage or by another condition that causes damage to nerves, such as diabetes.
Treatment
It is important to note that most patients with cervical radiculopathy get better over time and do not need treatment. For some patients, the pain goes away relatively quickly—in days or weeks. For others, it may take longer.
It is also common for cervical radiculopathy that has improved to return at some point in the future. Even when this occurs, it usually gets better without any specific treatment.
In some cases, cervical radiculopathy does not improve, however. These patients require evaluation and treatment.
Nonsurgical Treatment
Initial treatment for cervical radiculopathy is nonsurgical. Nonsurgical treatment options include:
Soft cervical collar: This is a padded ring that wraps around the neck and is held in place with Velcro. Your doctor may advise you to wear a soft cervical collar to allow the muscles in your neck to rest and to limit neck motion. This can help decrease the pinching of the nerve roots that accompany movement of the neck. A soft collar should only be worn for a short period of time since long-term wear may decrease the strength of the muscles in your neck.
Physical therapy: Specific exercises can help relieve pain, strengthen neck muscles, and improve range of motion. In some cases, traction can be used to gently stretch the joints and muscles of the neck.
Medications: In some cases, medications can help improve your symptoms.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs, including aspirin, ibuprofen, and naproxen, may provide relief if your pain is caused by nerve irritation or inflammation.
- Oral corticosteroids. A short course of oral corticosteroids may help relieve pain by reducing swelling and inflammation around the nerve.
- Steroid injection. In this procedure, steroids are injected near the affected nerve to reduce local inflammation. The injection may be placed between the laminae (epidural injection), in the foramen (selective nerve injection), or into the facet joint. Although steroid injections do not relieve the pressure on the nerve caused by a narrow foramen or by a bulging or herniated disk, they may lessen the swelling and relieve the pain long enough to allow the nerve to recover.
- These medications are reserved for patients with severe pain that is not relieved by other options. Narcotics are usually prescribed for a limited time only.

Facet joint injection in the cervical spine
Surgical Treatment
If after a period nonsurgical treatment does not relieve your symptoms, your doctor may recommend surgery. There are several surgical procedures to treat cervical radiculopathy. The procedure your doctor recommends will depend on many factors, including what symptoms you are experiencing and the location of the involved nerve root.
Learn more about surgery for radiculopathy: Cervical Radiculopathy: Surgical Treatment Options













