Low Back Pain
Table of Contents
- Introduction
- Anatomy
- Pathological Concepts of the Spine
- Diagnosis
- Diagnostic Tests
- Treatment Concepts
- Medications
- Physical Therapy
- Other Tips for a Healthy Back
Introduction
The spine is one of the most important parts of your body. Without it, you could not keep yourself upright or even stand up. It gives your body structure and support. It allows you to move about freely and to bend with flexibility. The spine is also designed to protect your spinal cord. The spinal cord is a column of nerves that connects your brain with the rest of your body, allowing you to control your movements. Without a spinal cord, you could not move any part of your body, and your organs could not function. Therefore, keeping your spine healthy is vital if you want to live an active life.
Anatomy
The parts of your spine and how they work
What exactly is the spine?
Your spine is made up of 24 small bones (vertebrae) that are stacked on top of each other to create the spinal column. Between each vertebra is a soft, gel-like cushion called a disc that helps absorb pressure and keeps the bones from rubbing against each other. Each vertebra is held to the others by groups of ligaments. Ligaments connect bones to bones; tendons connect muscles to bones. There are also tendons that fasten muscles to the vertebrae. The spinal column also has real joints (just like the knee or elbow or any other joints) called facet joints. The facet joints link the vertebrae together and give them the flexibility to move against each other.
Each vertebra has a hole in the centre, so when they stack on top of each other they form a hollow tube that holds and protects the entire spinal cord and its nerve roots. The spinal cord itself is a large collection of nerve tissue that carries messages from your brain to the rest of your body. For your body to function, you need your nerves. The spine branches off into thirty-one pairs of nerve roots. These roots exit the spine on both sides through spaces (neural foramina) between each vertebra.

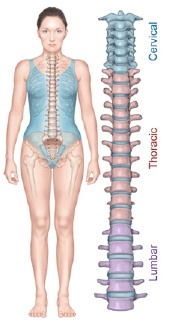
The spine itself has three main segments: the cervical spine, the thoracic spine, and the lumbar spine. The cervical is the upper part of the spine, made up of seven vertebrae (bones). The thoracic is the centre portion of the spine, consisting of 12 vertebrae. The lower portion of the spine is called the lumbar spine. It is usually made up of five vertebrae, however, some people may have six lumbar vertebrae. Having six vertebrae does not seem to cause a problem. Below the lumbar spine is the sacrum. The sacrum is a group of specialized vertebrae that connects the spine to the pelvis. During development (those nine months before birth), these vertebrae grow together (or fuse) creating one large "specialized" vertebral bone that forms the base of your spine and centre of your pelvis. The nerves that leave the spine in the sacral region control the bowel and bladder functions and give sensation (feeling) to the crotch area.
The normal spine has an "S"-like curve when looking at it from the side. This allows for an even distribution of weight. The "S" curve helps a healthy spine withstand all kinds of stress. The cervical spine curves slightly inward, the thoracic curves outward, and the lumbar curves inward. Even though the lower portion of your spine holds most of the body's weight, each segment relies upon the strength of the others to function properly.
Now, let' s look at the specific parts that make up your spine:
Vertebrae
The individual bones of the spine are the vertebrae. These are the building blocks of the spinal column. The vertebrae protect and support the spinal cord. They also bear most the weight put upon your spine. The body of each vertebra is the large, round portion of bone. The body of each vertebra is attached to a bony ring. When the vertebrae are stacked one on top of the other, this ring creates a hollow tube where the spinal cord passes through.
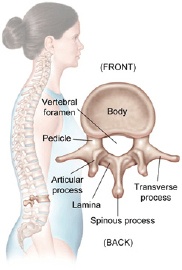
The bony ring attached to the vertebral body consists of several parts. First, the laminae extend from the body to cover the spinal canal, which is the hole in the centre of the vertebrae. Second, the spinous process is the bony portion opposite the body of the vertebra. You feel this part if you run your hand down a person's back. Then there are two transverse processes (little bony bumps), where the back muscles attach to the vertebrae. Finally, the pedicle is a bony projection that connects to both sides of the lamina.
The vertebra, like all bones, has an outer shell called cortical bone that is hard and strong. The inside is made of a soft, spongy type of bone called cancellous bone.
Intervertebral Disc
The intervertebral discs are flat, round "cushions" that act as shock absorbers between each vertebra in your spine. There is one disc between each vertebra. Each disc has a strong outer ring of fibres called the annulus, and a soft, jelly-like centre called the nucleus pulposus.
The annulus is the disc's outer layer and the strongest area of the disc. It also helps keep the disc's centre intact. The annulus is a strong ligament that connects each vertebra together.
The mushy nucleus of the disc serves as the main shock absorber. The nucleus is made up of tissue that is very moist because it has high water content. The water content helps the disc act like a shock absorber - somewhat like a waterbed mattress.
Facet Joint
The facets are the "bony knobs" that meet between each vertebra to form the facet joints that join your vertebrae together. There are two facet joints between each pair of vertebra, one on each side. They extend and overlap each other to form a joint between the neighbouring vertebra facet joints. Without the facet joints, you would not have flexibility in your spine, and you could only move in very straight and stiff motions.
The facet joints are what are known as synovial joints. A synovial joint, such as the knee or elbow, is a structure that allows movement between two bones. In a synovial joint, the ends of the bones are covered with a material called articular cartilage. This material is a slick, spongy material that allows the bones to glide against one another without much friction.
Surrounding the facet joint is a watertight sack made of soft tissue and ligaments. This sack creates what is called the "joint capsule". The ligaments are soft tissue structures that hold the two sides of the facet joint together. The ligaments around the facet joint combine with the synovium to form the joint capsule that is filled with fluid (synovial fluid). This fluid lubricates the joint to decrease the friction, just like oil lubricates the moving parts of a machine.
Neural Foramen
The neural foramen is the opening between every two vertebrae where the nerve roots exit the spine. The nerve roots travel through the foramen to reach the rest of your body. There are two neural foramina between each pair of vertebrae - one on each side. Without the foramen, nerve signals could not travel to and from the brain to the rest of your body. Without nerve signals, your body would not be able to function.
Spinal Cord and Nerve Roots
The spinal cord is a column of millions of nerve fibres that run through your spinal canal. It extends from the brain to the area between the end of your first lumbar vertebra and top of your second lumbar vertebra. At the second lumbar vertebra, the spinal cord divides into several different groups of fibres that form the nerves that will go to the lower half of the body. For a small distance, the nerves travel through the spinal canal before exiting out the neural foramen. This collection of nerves is called the cauda equina while it is still inside the spinal canal.
A protective membrane called the dura mater covers the spinal cord. The dura mater forms a watertight sack around the spinal cord and the spinal nerves. Inside this sack, the spinal cord is surrounded by spinal fluid.
The nerve fibres in your spinal cord branch off to form pairs of nerve roots that travel through the small openings (foramina) between your vertebrae. The nerves in each area of the spinal cord connect to specific parts of your body. Therefore, damage to the spinal cord can cause paralysis in certain areas and not others -- it depends on which spinal nerves are affected. The nerves of the cervical spine go to the upper chest and arms. The nerves in your thoracic spine go to your chest and abdomen. The nerves of the lumbar spine then reach to your legs, bowel, and bladder. These nerves coordinate and control all the body's organs and parts, and let you control your muscles.
The nerves also carry electrical signals back to the brain that allow you to feel sensations. If your body is being hurt in some way, your nerves signal the brain that you have been hurt. Damage to the nerves themselves can cause pain, tingling, or numbness in the area where the nerve travels.
Para spinal Muscles
The Para spinal muscles refer to the muscles next to the spine. They support the spine and are the motor for movement of the spine. Your joints allow flexibility and your muscles allow mobility. There are many small muscles in the back - each controlling some part of the total movement between all the vertebrae and the rest of the skeleton. These muscles can be injured directly, such as when you have a pulled muscle or muscle strain of the back muscles. The muscles can also cause problems indirectly, such as when the muscles are in spasm after injury to other parts of the spine.
When you experience a muscle spasm, it is because your muscle tightens up and will not relax. These spasms usually occur as a reflex - meaning that you cannot control the contraction of the muscles. When any part of the spine is injured, including: a disc, ligaments, bones, or muscles, the muscles automatically go into spasm to reduce the motion around the area. This protective mechanism is designed to protect the injured area.
When muscles are in spasm they produce too much of the chemical, lactic acid. Lactic acid is a waste product produced by the chemical reaction inside muscle cells that must occur to allow the muscle to contract. If the muscle cell cannot relax, too much lactic acid builds up inside the muscles. The build-up of lactic acid causes a painful burning sensation.
The main reason that lactic acid builds up inside the muscle cells is that when the muscles contract, the small blood vessels traveling through the muscles are pinched off (just like a tube pinched between your thumb and finger). When the muscle relaxes, the lactic acid is eventually washed away by fresh blood flowing into the muscle as the blood vessels open.
Spinal Segment
Back specialists sometimes look at a spinal segment to understand and explain how the whole spine works. A spinal segment is made up of two vertebrae attached together by ligaments, with a soft disc separating them. The facet joints fit between the two vertebrae, allowing for movement, and the neural foramen between the vertebrae allow space for the nerve roots to travel freely from the spinal cord to the body.
The spinal segment allows us to focus on the repeating parts of the spinal column to better understand what can go wrong with the various parts of the spine. Sometimes problems in the spine involve only one spinal segment, while other times the problems involve multiple segments.
Each spinal segment is like a well-tuned part of a machine. All the parts should work together to allow weight bearing, movement, and support. When all the parts are functioning properly, all spinal segments join to make up a remarkably strong structure called the spinal column. When one segment deteriorates to the point of instability, it can lead to problems at that segment causing pain and other difficulties.
Now that you know the parts of the spine, let's look at the spine itself, which has three main segments - the lumbar, thoracic, and cervical spines.
Lumbar Spine
The lowest part of the spine is called the lumbar spine. This area has five vertebrae. However, sometimes people are born with a sixth vertebra in the lumbar region. The base of your spine (sacrum) is a fusion of many bones, and when one of them forms as a vertebra rather than part of the sacrum, it is called a transitional (or sixth) vertebra. This occurrence is not dangerous and does not appear to have any serious side effects.
The lumbar spine's shape has what is called a lordotic curve. The lordotic shape is like a backwards "C". If you think of the spine as having an "S"-like shape, the lumbar region would be the bottom of the "S". The vertebrae in the lumbar spine area are the largest of the entire spine, so the lumbar spinal canal is larger than in the cervical or thoracic parts of the spine. Because of its size, the lumbar spine has more space for the nerves to move about.
Low back pain is a very common complaint for a simple reason. Since the lumbar spine is connected to your pelvis, this is where most of your weight bearing and body movement takes place. Typically, this is where people tend to place too much pressure, such as: lifting a heavy box, twisting to move a heavy load, or carrying a heavy object. Such repetitive injuries can lead to damage to the parts of the lumbar spine.
Thoracic Spine
The thoracic spine is made up of the middle 12 vertebrae of the spine. These vertebrae connect to your ribs and form part of the back wall of the thorax (the ribcage area between the neck and the diaphragm). This part of the spine has very narrow, thin intervertebral discs, so there is much less movement allowed between vertebrae than in the lumbar or cervical parts of the spine. It also has less space in the spinal canal for the nerves. The thoracic spine's curve is called kyphotic because of its shape, which is a regular "C"-shaped curve with the opening of the "C" in the front.
Cervical Spine
The cervical spine is made up of the first seven vertebrae in the spine. It starts just below the skull and ends just above the thoracic spine. The cervical spine has a lordotic curve (a backward "C"- shape) - just like the lumbar spine. The cervical spine is much more mobile than both other spinal regions - think about all the directions and angles you can turn your neck.
Unlike the rest of the spine, there are special openings in each vertebra in the cervical spine for the arteries (blood vessels that carry blood away from the heart), as well as the spinal canal that carries the spinal cord. The arteries that run through these openings bring blood to the brain.
Two vertebrae in the cervical spine, the atlas and the axis, differ from the other vertebrae because they are designed specifically for rotation. These two vertebrae are what allow your neck to rotate in so many directions, including looking to the side.
The atlas is the first cervical vertebra - the one that sits between the skull and the rest of spine. The atlas does not have a vertebral body, but does have a thick forward (anterior) arch and a thin back (posterior) arch, with two prominent sideways masses.
The atlas sits on top of the second cervical vertebra - the axis. The axis has a bony knob called the odontoid process that sticks up through the hole in the atlas. It is this special arrangement that allows the head to turn from side to side as far as it can. Special ligaments between these two vertebrae allow a great deal of rotation to occur between the two bones.
Though the cervical spine is very flexible, it is also very much at risk for injury from strong, sudden movements, such as whiplash-type injuries. This high risk of harm is due to the limited muscle support that exists in the cervical area, and because this part of the spine must support the weight of the head. This is a lot of weight for a small, thin set of bones and soft tissues to bear. Therefore, sudden, strong head movement can cause damage.
Pathological Concepts of the Spine
Back pain can be caused by several spinal conditions, and below are descriptions of various causes of discomfort:
Mechanical versus Compressive pain
Sometimes it is useful for back specialists to understand back problems by dividing the problems into different categories. One way to look at back pain is to divide problems into two large categories -- mechanical back pain and compressive back pain.
Mechanical pain is often called back strain because is linked with the movement, or "the mechanics" of the spine. This type of pain occurs when injury to the spine's discs, facet joints, ligaments, or muscles results in inflammation. It is called mechanical pain because it relates to the mechanics of your spine. The more you use the back, the more it hurts. This pain can be caused by many conditions in the spine. These conditions include: fractures of the vertebra, muscle strains in the Para spinal muscles, ligament injures in the spine, and wear and tear of the spine's joints and discs.
Compressive pain is a result of pressure or irritation on the spinal cord, or nerves that leave the spine. For example, if an intervertebral disc herniates (usually called a ruptured disc) and pushes into the spinal canal, it can cause problems with the nerve. Usually this pressure or irritation causes pain, numbness, and muscle weakness where the nerve travels.
Each part of the spine can cause pain. It can be helpful to understand which part of the spine is causing your back pain and whether the pain is from a compressive or mechanical type problem.
Arthritis Pain
The term arthritis means inflammation of the joints. Arthritis of the spine usually refers to a condition where there is inflammation of the facet joints between the vertebrae. The pain that results from arthritis is usually the mechanical type of back pain. If bone spurs develop due to the arthritis and begin rubbing on the spinal nerves, there can also be compressive type pain produced as well. There are two types of arthritis: systemic inflammatory arthritis, and wear-and-tear arthritis. A systemic type of arthritis is a disease process that affects all the joints of the body - such as rheumatoid arthritis. Many arthritis type diseases affect the connective tissues of the body. These diseases cause inflammation of the joint tissues and destruction of the joints. The joints of the spine may be involved in systemic types of arthritis because the facet joints are made up of the same tissues as any other joint. Therefore, diseases that attack joint tissues also attack the facet joints.
Wear-and-tear arthritis, or osteoarthritis, can result from many things. It can come from a single injury that damages the joint. It can also result from a lifetime of overuse of different joints that damage the joint a little bit at a time. Doctors are now beginning to realize that osteoarthritis also runs in families. Something about the genetic makeup of different individuals makes them more prone to develop osteoarthritis of various joints.
Osteoarthritis is caused by a permanent breakdown of the articular cartilage inside the affected joint. Articular cartilage is the material inside the joint that cushions the bones of the joints from impact and allows smooth, gliding motions. Because damaged cartilage cannot repair itself, it begins to fray, making it less flexible and more prone to injury. Over time, the cartilage can wear away completely, causing the bony surfaces of the joint to rub directly against each other. Eventually the joint becomes worn away and bone spurs develop around the joint.
Facet Joint Syndrome
Sometimes the facet joints are the main cause of back pain. In many cases, the facet joints are at least part of what is causing your back pain. When your doctor thinks the facet joints are a major source of your pain, he may use the term "facet joint syndrome". Facet joint degeneration, or osteoarthritis, can be caused by a combination of aging, pressure overload of the facet joints, and injury.
Pressure overload on the facet joints is probably caused by degeneration of the intervertebral disc. As the discs’ degenerate, they wear down and begin to collapse. This narrows the space between each vertebra. This narrowing of the space between each vertebra affects the way the facet joints line up. When this occurs, it places too much pressure on the articular cartilage surface of the facet joint. The excessive pressure leads to damage of the articular surface and eventually the cartilage begins to wear away.
When facet joint arthritis gets bad enough, the cartilage and fluid that lubricate the facet joints are eventually destroyed as well, leaving bone rubbing on bone. Bone spurs begin to form around the facet joints. When bone spurs develop, they can take up space in the foramen (the opening between vertebrae where nerve roots exit the spine) and press into nerve roots. As the bone spurs begin to grow larger, they can eventually extend into the spinal canal itself. This leads to narrowing of the spinal canal (spinal stenosis).
Pinched Nerve (Radiculopathy)
Radiculopathy is the medical term used to describe a "pinched nerve" in the spine. A radiculopathy occurs when a nerve is irritated by something that is either rubbing on the nerve or pressing on the nerve. In some cases, such as a herniated (or ruptured) disc, there may also be a chemical reaction irritating the nerve. Chemicals released from the inside of the disc seem to irritate nerve tissue, causing pain and inflammation of the nerve.
Abnormal pressure or irritation on a nerve causes several problems. First, there is numbness in the area where the nerve usually provides sensation, or feeling. For example, if the nerve usually ends in the side of the foot and supplies sensation to that area, it will have decreased feeling, and often pain.
The key to understanding a radiculopathy is understanding that your brain cannot tell where the problem really is. While the irritation or pressure on the nerve may be in your back, your brain thinks the pain is coming from your foot. In addition, the muscles that the nerve usually controls will not work right. You will usually have weakness in the muscles, and the reflexes controlled by the muscles will not work. Therefore, doctors always check reflexes. The body has a pretty standard wiring diagram. By determining which reflexes are not working, the doctor can usually tell which nerve is involved with the problem.
Things that can cause a radiculopathy include: herniated discs, bone spurs, tumours that are growing into the nerves, and fractures that put pressure on the nerves.
Sciatica
The term sciatica refers to a certain type of radiculopathy that occurs in the leg. It is called sciatica because it describes the radiculopathy that occurs when one or more of the nerves that make up the large sciatic nerve are irritated or pinched. Therefore, sciatica is not any different than a pinched nerve anywhere else in the spine. It simply has its own name because it is common. It also occurs in the lumbar spine, the most common site of spinal nerve irritation.
Sciatica is used to describe the pain that travels from the sciatic nerve in the lumbar region into your buttocks, back of the thighs, and sometimes calf and foot. The pain is typically caused by irritation of the nerve roots that join outside the spine to make up the sciatic nerve. Conditions that can cause sciatica are: herniated discs, bone spurs, cancerous tumours that are growing into the nerves, and fractures that put pressure on the nerves.
Spinal Cord Pressure
We have seen how individual nerve roots are affected by pressure and irritation -- but what about the spinal cord itself? Pressure on the spinal cord typically results from a condition called stenosis. Stenosis means narrowing of an opening or tube - in this case the spinal canal.
Spinal Stenosis
Spinal stenosis is a term commonly used to describe a narrowing of a portion of the spinal canal. Stenosis can occur in all areas of the spine, but it is most common in the cervical and lumbar spine. There can often be narrowing of most of the lumbar spinal canal and of several segments of the cervical spine. Each behaves somewhat differently.
Although there is some space between the spinal cord and the edges of the spinal canal, this space can be reduced by many conditions. Bone and tough ligaments surround the spinal canal. This tube cannot expand if the spinal cord or nerves require more space. If anything begins to narrow the spinal canal, the risk of irritation and injury of the spinal cord or nerves increases. Some conditions that can lead to narrowing of the spinal canal include: infection, tumours, trauma, herniated disc, arthritis, thickening of ligaments, growth of bone spurs, and disc degeneration.
Spinal stenosis usually occurs in older people after years of wear and tear or degeneration of the spine. This wear and tear results in changes in the structures around the spinal canal, such as thickening of the large ligaments that connect the vertebra together, bone spurs around the facet joints and disc space, and bulging of the discs themselves. These changes push into the spinal canal, making the tube of the spinal canal smaller. Eventually, there is not enough space in the spinal canal for the nerve to comfortably fit without causing too much pressure. Stenosis can also develop because of injuries, infections, or tumours. Some people even have a narrow spinal canal from birth, and this abnormality leads to symptoms of stenosis.
The narrowing of the spinal canal can lead to irritation of the nerves of the spine. This can cause pain and problems with the nerves not working right. The lack of space can also cause the supply of blood and oxygen to the spinal cord to be reduced. When the spine needs more blood flow during increased activity, the blood vessels may not be able to swell to get more blood to the spine. This can lead to numbness and pain in the affected nerves. The nerves also lose some of their mobility when the space available to them is reduced. This leads to irritation and inflammation of the nerves.
Other symptoms of spinal stenosis include: a sensation of heaviness, weakness, and pain when walking or standing for a long period. With rest, these symptoms often disappear. These symptoms occur because the nerve roots are being tampered with, upsetting the normal signals that travel from the brain to the body. Irritation of the nerves in the spinal canal is worse when standing or walking because of the mechanical compression and stretching of the nerves.
Segmental Spinal Stenosis
Segmental spinal stenosis is a narrowing of the spinal canal in a segmented, or specific, area. Sometimes the stenosis only occurs in a small area of the spine, such as an area where there is a combination of bone spurs from the facet joints in the back of the spinal canal and a bulging disc in the front of the spinal canal. This results in narrowing of that one area of the spine.
Segmental stenosis can occur in both older and younger people. The symptoms of segmental spinal stenosis are like other conditions of the spine. Segmental spinal stenosis can affect the nerve roots that leave the spine at the area where the segmental stenosis occurs. These nerves can become irritated, causing pain, numbness, and weakness in the area the nerve travels. There can also be pressure on the rest of the spinal nerves that must travel through the narrowed area of the spinal canal.
Discogenic Pain is a term back specialists use when referring to pain caused by a damaged intervertebral disc. A degenerating disc may cause pain of the mechanical type. As the disc begins to degenerate, there is some evidence that the disc itself becomes painful. Movements that place stress on the disc can result in back pain that appears to come from the disc. This is like any other body part that is injured, such as a broken bone, or even a cut in the skin. When these types of injuries are held still, there is no pain. However, if you move a broken bone, or the skin around a cut, it causes pain.
Discogenic pain usually causes pain felt in the lower back. It may also feel like the pain is coming from your buttock areas and even down into the upper thighs. The experience of feeling pain in an area away from the real spot causing the pain is common in many areas of the body, not just the spine. Examples include: a person who has gallstones may feel the pain in their shoulder; or a person experiencing a heart attack may feel pain in the left arm. This is called radiation of the pain. It is very common for pain produced by spine problems, such as disc problems, to be felt in different areas of the body, including the back itself.
Bulging Disc
Bulging discs are common in both young adults and older people. They are not cause for panic. In fact, abnormalities that show up on MRIs, such as bulging or protruding discs, are seen at high rates in patients both with and without back pain. Most likely, some discs begin to bulge as a part of the aging process, and the degeneration process of the intervertebral disc. A bulging disc is not necessarily a sign that anything serious is happening to your spine.
A bulging disc becomes important when it bulges enough to cause narrowing of the spinal canal. If there are bone spurs present on the facet joints behind the bulging disc, the combination may cause narrowing of the spinal canal in that area. This is sometimes referred to as segmental spinal stenosis.
Herniated Disc
A herniated disc s occurs when the intervertebral disc's outer fibres (the annulus) are damaged and the soft inner material of the nucleus pulposus ruptures out of its normal space. If the annulus tears near the spinal canal, the nucleus pulposus material can push into the spinal canal. This can cause too much pressure on the spinal cord and nerve roots. There is also some evidence that the nucleus pulposus material causes a chemical irritation of the nerve roots. Both the pressure on the nerve root and the chemical irritation can lead to problems with how the nerve root works. The combination of the two can cause pain, weakness, and/or numbness in the area of the body to which the nerve travels. For this reason, a herniated disc usually causes pain of the compressive type. Sometimes a herniated disc is referred to as "slipped disc", though the disc does not actually slip.
Herniated discs are common in the lumbar spine because of all the pressure it supports. A herniated lumbar disc often produces sciatica. This is a condition where the lower back pain and numbness radiates down the back of the leg, side of the calf, and possibly into the side of the foot. You may not necessarily have much back pain. The exact area where you will feel numbness depends on the nerve root that is affected; the numbness could be in the inner ankle, big toe, heel, outer ankle, outer leg, or a combination of them. Your doctor can use this information to get an idea which nerve is affected.
Pressure on the nerve root can cause the parts of the nerve that control the muscles not to work properly. This can result in weakness of some muscles and may change the reflexes in certain areas. Again, your doctor can use this information to try to determine which nerve is involved.
The same is true for the neck. A problem stemming from the neck may result in pain that is perceived in the arm or hand. However, a herniated disc is much less common in the thoracic spine. This is likely because the discs are much thinner and there is less material in the nucleus pulposus to rupture into the spinal canal. HOWEVER, if a herniated disc does occur in the thoracic spine, it can be much more serious than in the lumbar spine. The thoracic spine has very little extra room in the spinal canal. In addition, a herniated disc in the thoracic spine puts pressure on the spinal cord - not just a few nerve roots. Too much pressure on the spinal cord from a herniated thoracic disc can lead to total paralysis from the waist down.
Just because a disc has herniated does not necessarily mean that you will need to undergo surgery. In most cases, a herniated disc can be treated without surgery. The treatment of a herniated disc depends on the symptoms. It also depends on whether the symptoms are getting steadily worse – or whether they are getting better. If the symptoms are getting steadily worse, your doctor may be more likely to suggest surgery. If the symptoms are getting better, your doctor may suggest watching and waiting to see if the symptoms go away. In many cases, the initial problems due to a herniated disc completely resolve over several weeks to months.
In rare cases, a herniated disc in the lumbar spine area can be so large that it fills the entire spinal canal in the area where it ruptures. When the spinal canal fills with disc material, it may place a great amount of pressure on the nerves. If this occurs in the lower spine, it can lead to a condition called "cauda equina syndrome". This problem can lead to permanent paralysis of the muscles that control your bowels and bladder. If you lose control over your bladder or bowels, you should contact your health care provider immediately. These symptoms require immediate medical attention.
Degeneration of the Intervertebral Disc
The process of degeneration of the intervertebral disc causes many problems in the spine. Everything you do during the day - once you stand upright - begins to test the spine's ability to support your body weight. Over time, these repeated daily stresses and minor injuries can add up and begin to affect the discs in your spine. Minor injuries to a disc may occur and not cause pain at the time. However, as they add up, the disc eventually begins to suffer from the wear and tear – it begins to degenerate.
There is an intervertebral disc between each of your vertebra. The intervertebral discs are designed to absorb pressure and keep the spine flexible by acting as cushions during body movement. The discs work similarly to shock absorbers. They are like cushions in running shoes; without them, a jogger would feel every pound on the pavement, and the feet would soon tire out. Without the cushion effect of the discs, the vertebrae in your spine would probably fracture or break. Bones cannot sustain high stress repeatedly without being cushioned.
A healthy intervertebral disc has a great deal of water in the nucleus pulposus - the centre portion of the disc. The water content gives the nucleus a spongy quality and allows it to absorb spinal stress. Excessive pressure or injuries to the disc can cause the injury to the annulus - the outer ring of tough ligament material that holds the vertebrae together. Generally, the annulus is the first portion of the disc that seems to be injured. Small tears show up as in the ligament material of the annulus. These tears heal by scar tissue. The scar tissue is not as strong as normal ligament tissue. Over time as more scar tissue forms, the annulus becomes weaker. Eventually this can lead to damage of the nucleus pulposus. The nucleus begins to lose its water content due to the damage - it begins to dry up.
Because of water loss, the discs lose some of their ability to act as a cushion. This can lead to even more stress on the annulus and still more tears as the cycle repeats itself. As the nucleus loses its water content it collapses, allowing the two vertebrae above and below to move closer to one another. This results in a narrowing of the disc space between the two vertebrae. As this shift occurs, the facet joints located at the back of the spine must shift. This shift changes the way the facet joints work together and can cause problems in the facet joints as well.
Bone spurs, sometimes called osteophytes, may also form around the disc space. These bones spurs can also form around the facet joints. This is thought to be due to the body's response to try to stop the excess motion at the spinal segment. The bone spurs can become a problem if they begin to grow into the spinal canal and press into your spinal cord and nerves. This condition is called spinal stenosis.
Segmental Instability of the Spine
Each spinal segment is like a well-tuned part of a machine. All the parts should work together to allow weight bearing, movement, and support. A spinal segment is composed of two vertebrae attached together by ligaments, with a soft disc separating them. The facet joints fit between the two vertebrae, allowing for movement, and the foramen between the vertebrae allows space for the nerve roots to travel freely from the spinal cord to the body. When all the parts are functioning properly, the spinal segments join to make up a remarkably strong structure called the spine. When one segment deteriorates to the point of instability, it can lead to localized pain and difficulties.
Segmental instability occurs when there is too much movement between two vertebrae. The excess movement of the vertebrae can cause pinching or irritation of nerve roots. It can also cause too much pressure on the facet joints, leading to inflammation of facet joints. It also may cause muscle spasms as the Para spinal muscles try to stop the spinal segment from moving too much. The instability eventually results in faster degeneration of the spine in this area.
It is hard to determine which problem comes first in segmental instability. In some cases, degeneration of the disc begins the process. Once the disc is no longer able to function normally, the degeneration process of ALL parts of the spinal segment begins. As the disc continues to degenerate, the facet joints become arthritic, bone spurs form around the joints, and the segmental instability gets worse. This cycle continues.
Diagnosis
Before a health care professional can diagnose your condition and design a treatment plan, a complete history and physical examination are necessary. There are so many possible internal causes of pain; it is important to determine what is and is not causing the problem. After the physician has a better idea of what is attributing to your discomfort, diagnostic tests of some sort may be recommended.
History
First, you will be asked for a complete physical history of your condition. This may begin by filling out a written form that asks you several questions relating to your pain. The more information you share with the provider, the easier your problem will be to diagnose. Your physical history is important because it helps your doctor understand: when the pain began, anything that could have caused an injury, your lifestyle, physical factors that might be causing the pain, and your family history of similar problems. After reading through your written history, your physician will ask more questions that relate to the information you have given.
Some typical questions include:
- When did the pain begin?
- Was there an injury that could be related to the pain?
- Where do you feel the pain? What is the intensity?
- Does the pain radiate to other parts of the body?
- What factors make the pain feel better or worse?
- Have you had problems with your bladder or bowels?
- Is there a history of osteoporosis in your family?
Physical Examination
After taking your history, the physician will give you a physical examination. This allows the doctor to rule out possible causes of pain and try to determine the source of your problem. The areas of your body that will be examined depend upon where you are experiencing pain - neck, lower back, arms, legs, etc.
The following are some of the things that are checked in a typical exam:
- Motion of Spine and Neck - Is there pain when you twist, bend, or move? If so, where? Have you lost some flexibility?
- Weakness - Your muscles will be tested for strength. You might be asked to try to push or lift your arm, hand, or leg when light resistance is put against them.
- Pain - The doctor may try to determine if you have tenderness of certain areas.
- Sensory Changes - Can you feel certain sensations in specific areas of the feet or hands?
- Reflex Changes - Your tendon reflexes might be tested, such as under the kneecap and under the Achilles tendon on your ankle.
- Motor Skills - You might be asked to do a toe or heel walk.
- Special Signs - The physician will also check for any "red flags" that could indicate something other than spinal/vertebrae problems. Some signs of other problems include tenderness in certain areas, a fever, an abnormal pulse, chronic steroid use (leads to loss of bone mass), or rapid weight loss.
Diagnostic Tests
You may be asked to take a variety of diagnostic tests. The tests are chosen based upon what your physician suspects is the cause of your pain. These are the most common diagnostic tests:
X-rays
An X-ray is a painless process that uses radioactive materials to take pictures of bone. If your doctor suspects vertebral degeneration, X-rays can be used to verify: a decrease in the height of space between discs, bone spurs, nerve bundle sclerosis (hardening), facet hypertrophy (enlargement), and instability during flexion or extension of limbs. X-rays show bones, but not much soft tissue, so they will be used if fractures, infections, or tumours are suspected.
During X-rays, you will be asked to lie very still on a table and hold certain positions while photographs are taken of your spine.
MRI Scan (Magnetic Resonance Imaging)
The MRI scan is a fairly new test that does not use radiation. By using magnetic and radio waves, the MRI creates computer-generated images. The MRI can cut through multiple layers of the spine and show any abnormality of soft tissues, such as nerves and ligaments. The test also can be used to verify: loss of water in a disc, facet joint hypertrophy (enlargement), stenosis (narrowing of spinal canal), or a herniated disc (protrusion or rupture of the intervertebral disc).
During an MRI test, you lie on a table that slides into a machine with a large, round tunnel. The machine's scanner then takes many pictures that are watched and monitored by a technician. Some newer MRI machines, called Open MRIs, are likely to be more comfortable for patients who experience claustrophobia. The procedure takes 30-60 minutes.
CAT Scans (Computer Assisted Tomography)
The CAT scan is an X-ray test that is like both the MRI and a regular X-ray, because it can show both bones and soft tissues. CAT scans are also able to produce X-ray "slices" taken of the spine, allowing each section to be examined separately. The scan forms a set of cross-sectional images that can show disc problems and degeneration of bones, such as bone spur formation or facet hypertrophy (enlargement). CAT scan images are not as clear as either X-rays or an MRI. To make the soft tissues easier to see, the CAT scan is often combined with a myelogram.
Like an MRI, with a CAT scan you will lie on a table that slides into a scanner. The scanner is essentially an X-ray tube that rotates in a circle taking many pictures. The procedure takes 30-60 minutes.
Myelogram
A myelogram is an older test that is used to examine the spinal canal and spinal cord. During this test, a special X-ray dye is placed into the spinal sac. This will require a spinal tap to be performed by your doctor. This procedure is performed by inserting a small needle in the lower back and into the spinal canal. Through the needle, dye is injected which mixes with the spinal fluid. The dye shows up on X-rays. Therefore, when the X-ray is taken, the dye outlines the spinal cord and nerve roots so that disc and bone spur problems can be seen.
To conduct the myelogram, the patient lies on a tilting table. As the table tilts, the movement of the dye shows the outline of the spinal sac. X-rays are taken as the patient is titled to show the flow of the dye through the spinal region, helping doctors determine if there is any unusual indentation or an abnormal shape. This indentation could be from a herniated or bulging disc, lesions, tumours, or injury to the spinal nerve roots. The myelogram is often combined with a CAT scan to get a better view of the spine in cross section.
In many cases, the MRI has replaced both the myelogram and the CAT scan. Sometimes the myelogram still shows the problem better than the MRI, but today it is used less frequently than the MRI.
Bone Scan
A bone scan can be used to locate any problem areas of the spine. The bone scan works by injecting a radioactive chemical, sometimes called a "tracer", into the bloodstream through an IV. The chemical will attach itself to areas of bone that are undergoing rapid changes. Over a period of several hours, a lot of the tracer accumulates in the problem area(s).
A special camera is then used to take pictures of the skeleton. The chemical tracer is radioactive, and therefore sends out radiation that can be captured by the camera. Specific problem areas show up on the film as dark spots or "hotspots".
A bone scan is very useful when it is unclear exactly where the problem is in the skeleton. The ability to take a picture that lights up the area where the problem seems to be coming from allows the doctor to pinpoint where to look next. After locating the problem areas, other tests can be done to show more aspects of those specific spots. The bone scan can identify problem areas such as bone tumours and compression fractures. A bone scan can also be used to determine bone density and the bone-thinning condition of osteoporosis.
EMG/SSP (Electro diagnostic Study)
An electromyogram (EMG) is a test that looks at the function of the nerve roots leaving the spine. The test is done by inserting tiny electrodes into the muscles of the lower extremity. By looking for abnormal electrical signals in the muscles, the EMG can show if a nerve is being irritated or pinched as it leaves the spine. Think of how you test the wiring on a lamp. If you place a working bulb into the lamp, and the bulb lights up, you assume that the wiring is okay. However, what if the bulb does not light up? You can safely assume that something is probably wrong with the wiring, like the lamp is unplugged, or a short circuit has occurred. By using the muscles like the light bulb in the lamp, the EMG can determine the condition of the nerves that supply those muscles, just like the wiring on the lamp. If the EMG machine finds that the muscles (the light bulb) are not working properly, the doctor can assume that the nerves (the wiring) must be getting pinched somewhere.
Facet Joint Block
Like any joint in the body, facet joints can cause pain if they are irritated or inflamed. The facet joint block is a procedure where a local anaesthetic medication (such as lidocaine or Novocain) is injected into the facet joint. This same type of medication is used by a dentist to numb your jaw, or a doctor to sew up a laceration. The lidocaine numbs the area around the facet joint. If all your pain goes away, the doctor can assume that the facet joint is a problem.
Laboratory Tests
Further lab tests may be done to check for problems that are not related to deterioration of the spine. Other testing can help determine the presence of serious problems such as: an infection, arthritis, cancer, or an aortic aneurysm. The most frequent lab test is blood sampling.
Spinal Tap
A spinal tap is done to get a sample of the cerebrospinal fluid that surrounds the spinal cord. The fluid is usually very clear. It contains proteins, sugar, and other substances that can be found in blood. It typically does not contain red blood cells or many white blood cells. A spinal tap checks the pressure and content of the fluid. Signals that there may be problems include: evidence of bleeding, an increase in white blood cells (infection fighting cells, dead cells are "pus"), an increase in protein level, or inflammation. This could mean infection, tumours, or a haemorrhage around the brain or spinal cord. To obtain the fluid sample, a needle will be inserted into the spinal canal in the lumbar region.
Discogram
A discogram is an X-ray examination of the intervertebral discs. This test is used to determine which disc(s) are damaged and if surgery is necessary. The test is performed by injecting dye into the centre of the injured disc(s). The dye makes the disc clearly visible on X-ray film and a fluoroscope screen. This test is better than an X-ray or myelogram for determining if there is a disc problem. The dye helps the physician make an accurate diagnosis. A simple X-ray shows only the vertebrae, and a myelogram is best for assessing the spinal canal.
With a discogram, you will be given medication to help you relax, then a local anaesthetic. The procedure usually lasts about 40 minutes.
Treatment Concepts
On your first visit to a back specialist, the initial decision that must be made is exactly how serious the problem is. Some problems need immediate attention - possibly even surgery. However, the clear majority of back problems do not require surgery. Once the most likely cause of your problem has been determined (your diagnosis has been made), you and your health care provider can decide on a treatment plan.
A variety of treatment options exist for different types of back pain, and in most cases, simple therapies such as mild pain medications and rest, are effective in relieving the immediate pain. The overall goal of treatment is: to make you comfortable as quickly as possible, to design a program to reduce further degeneration, and to get you back to normal activity as soon as possible. The more
you know about how your back works and what you can do to prevent further injury, the more effective your program will be. Below are descriptions of the most common forms of treatment, along with a brief explanation of what each is designed to do.
"Conservative" Treatment
Back specialists often use the term "conservative treatment" to describe any treatment option that does not involve surgery. Therefore, you may hear, or read in your records, that your provider is recommending a course of conservative treatment for your back problem. Treatment for your back problem may be as simple as reassuring you that it is not a serious problem and doing nothing but watching and waiting. However, usually anyone who has a back problem that becomes symptomatic should consider some preventive measures. This usually means that you should learn more about how to protect your back and consider beginning exercises to strengthen your back. These exercises can be quick and easy to do, do not require any special equipment, and can help prevent problems later.
A variety of treatment options exist for back pain that is the result of degeneration (wear and tear) on the parts of the spine. In most cases, simple therapies such as mild pain medications and rest are effective. The goal of treatment is to make you feel comfortable, reduce further degeneration, and get you back to normal activity as quickly as possible. As a last resort, and only if all other conservative treatments fail, surgery might be considered.
Specific Rest
Immediately after a back injury, rest is often all your back needs to feel better. Rest is used to take the pressure off your spine and the muscles around your spine. You should rest in a comfortable position on a firm mattress. Placing a pillow under your knees can also help relieve pain. Do not stay in bed for several days! Bed rest for more than two or three days can weaken the back muscles, making the problem worse instead of better. Even though you may still feel some pain, a gradual return to normal activities is good for your muscles. In most cases of sudden back pain, the sooner you start moving again, the sooner your back pain will resolve. If you are sent to see a physical therapist, the first few days may be spent educating you on ways to take stress off the back while remaining as active as possible. Short periods of rest combined with brief exercises designed to reduce your pain may be suggested.
Medications
Mild pain medications can reduce inflammation and pain when taken properly. Medications will not stop degeneration, but they will help with pain control.
Aspirin
Aspirin compounds are over-the-counter pain relievers that can help relieve minor pain and back ache. The main potential side effect of aspirin is the development of stomach problems, particularly ulcers with or without bleeding. You should not take aspirin if you are pregnant. In fact, you should not take any medication unless you have discussed the medication with your obstetrician.
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs)
NSAIDs include over-the-counter pain relievers such as ibuprofen or naproxen. These medications once were only available by prescription. NSAIDs are very effective in relieving the pain associated with muscle strain and inflammation. They block the inflammatory response in joints. However, be aware that NSAIDs can decrease renal function if you are an older patient. Excessive use can lead to kidney problems. Again, do not take them if you are pregnant.
Non-narcotic Prescription Pain Medication
Non-narcotic analgesics (the term analgesics means "pain relievers") address pain at the point of injury. Analgesics are ideal in the treatment of mild to moderate chronic pain. Tylenol and aspirin are the most widely used over-the-counter analgesics. Medications that are analgesics and require a prescription from the doctor include NSAIDs such as: carprofen, fenoprofen, ketoprofen, and sulindac. To reduce any side effects: do not lie down for 15 to 30 minutes after taking medication, avoid direct sunlight, wear protective clothing, and sun block. Avoid using these medications if you are pregnant, have recurrent ulcers, or liver problems.
Narcotic Pain Medications
If you experience severe pain, your health provider might prescribe a narcotic pain medication such as codeine or morphine. Narcotics relieve pain by acting as a numbing anaesthetic to the central nervous system. The strength and length of pain relief differs for each drug. Narcotics can cause related side effects such as nausea, vomiting, constipation, and sedation or drowsiness. These side effects are predictable and can often be prevented. Common preventative measures include: not taking sleeping aids or antidepressants in conjunction with narcotics, avoiding alcohol, increasing fluid intake, eating a high fibre diet, and using a fibre laxative or stool softener to treat constipation. Remember that narcotics can be addictive if used excessively or improperly.
Muscle Relaxants
If you are having muscle spasms, muscle relaxants can help relieve pain, but they are only shown to be marginally effective. They also have a significant risk of drowsiness and depression. Long-term use is not suggested; only three to four days is typically recommended.
Antidepressants
Back pain is a common symptom of depression and could be an indicator of its presence. Antidepressants can relieve emotional stress that leads to symptoms of back pain. An important fact to note - it seems that the same chemical reactions in the nerve cells that trigger depression also control the pain pathways in the brain. Some Antidepressant medications seem to reduce pain, probably because they affect this chemical reaction in the nerve cells. Some types of antidepressants also make rather good sleeping medications. If you are having trouble sleeping due to your back pain, your doctor may prescribe an antidepressant to help you get back to a normal sleep routine. Antidepressants can have several side effects such as: drowsiness, loss of appetite, constipation, dry mouth, and fatigue.
Epidural Steroid Injections (ESI) - Nerve Blocks
These can be used to relieve the pain of stenosis and irritated nerve roots, as well as to decrease inflammation. Injections can also help reduce swelling from a bulging or herniated disc. The steroid injections are a combination of cortisone (a powerful anti-inflammatory steroid) and a local anaesthetic that are given through the back into the epidural space. Epidural steroid injections are not always successful in relieving symptoms of inflammation. They are used only when conservative treatments have failed.
Physical Therapy
If physical therapy is recommended, your treatment plan could include one or more types of therapy:
Modalities - alternating heat and ice, massage, ultrasounds, and electric stimulation
Bracing - ranging from a simple corset to a rigid plastic body jacket
Flexibility and Strength Training - this is achieved through exercises, posture retraining, stretching, etc.
Pool Therapy - unloads spinal pressure because of the decrease in gravity provided by the water
Posture Training - learning how to stand, sit, and move properly; incorrect posture can contribute to back pain
Other Tips for a Healthy Back
Pay Attention to your Body: If something you are doing causes your back to hurt, stop and rest or stop altogether. Whether it is an exercise, prolonged sitting, bending, or twisting, listen to your body's signals. Pain is a warning. Discuss the activity with your doctor or physical therapist before proceeding.
Sit and Sleep Comfortably: Be sure that your back and neck are properly supported when you sit or sleep. When you sit, make sure your lower back is supported. Talk to your health care provider about choosing an appropriate mattress and pillow. You can upset the alignment of your spine if a mattress is too soft, or a pillow too high.
Lose Weight: If your weight is causing excessive pressure to your spine, weight loss can reduce your discomfort.
Lift Properly: Do not lift heavy loads by placing the pressure on your lower back. Use your legs to lift, and always bend your knees so your arms are at the same level as the heavy object you plan to lift. This simple technique will save your back unnecessary wear and tear.
Avoid Osteoporosis: Talk with your physician about combating the effects of osteoporosis – bone thinning. Possible treatments include weight bearing exercise, adequate calcium and vitamin D, and hormone replacement therapies.













